Not just a disease of the elderly
You, Your Child & Arthritis is a valuable resource for families of children with juvenile arthritis (JA). This endorsed guide provides the information parents/caregivers need to understand their child’s disease and to feel comfortable caring for them as well as the different types of juvenile arthritis, current treatments and learning to cope with a child who has a chronic disease.
Understanding JA
Many people mistakenly think arthritis is just a disease of the elderly, but the statistics tell a different story. About three in one thousand Canadian children have juvenile arthritis, which makes it more common than most chronic childhood diseases. You may have heard of the medical term “juvenile idiopathic arthritis” and wondered what it means. “Idiopathic” simply means “unknown.” This word is used when other illnesses or triggers known to cause arthritis have been ruled out as the cause of a child’s arthritis. Throughout this guide, Juvenile Arthritis (JA) will be used for the sake of simplicity. The term Juvenile Arthritis is an umbrella term that refers to seven different types of JA
(see below).
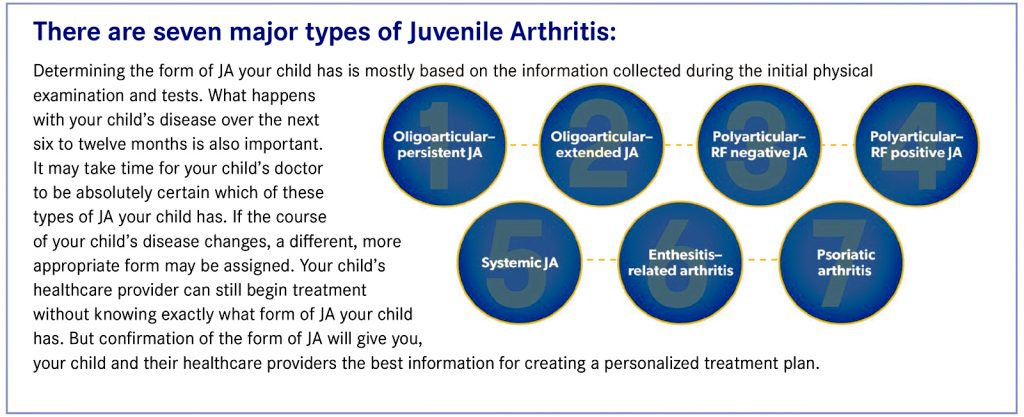
While there is no cure, treatment options exist and can be effective. Once a child has been diagnosed, parents will decide on the overall treatment plan with a child’s doctor and arthritis healthcare team. This plan will include medication and rehabilitation therapy. The therapy program is one of the cornerstones of treatment: exercise helps prevent the loss of joint movement and encourages normal growth. Although JA may cause joint damage, the bones and cartilage of growing children have amazing abilities to heal.
The medications prescribed by a child’s doctor act to reduce or stop joint swelling, pain and stiffness. They can also prevent joint damage and make a child’s therapy program easier to do. The type and strength of medication will depend on the child’s diagnosis. Children who are well monitored and follow the recommended treatment provided by a healthcare team have the best outcomes overall. The majority of children with JA are able to participate in normal activities and have a bright future.
What is Arthritis?
The word arthritis (arthro = joint, itis = inflammation) is a term referring to inflammation of the joint. Inflammation is a medical term that describes swelling, heat and redness which causes pain and, when in the joints, can also cause stiffness. In the case of inflammatory arthritis, like JA, an individual’s own immune system attacks tissue in the lining of the joint, causing it to feel warm, stiff, swollen and, often, painful.
In the joint space between two bones, there is a lining called synovium, which produces a fluid that lubricates and nourishes the joints. The ends of the bones at the joint are covered with a substance called cartilage, which allows bone ends to glide smoothly across each other. In JA, and other forms of inflammatory arthritis, an imbalance in the immune system causes the synovium to become inflamed and thickened, leading to the production of extra fluid. This fluid contains inflammatory cells which secrete proteins and chemicals of inflammation. This causes increased warmth, stiffness, swelling and pain in the affected joint. If left untreated, the inflammation can damage the cartilage and the underlying bone.
Arthritis can involve almost any part of the body, most often affecting large joints such as knees, ankles, wrists and elbows. It can also be found in small joints such as the fingers and toes. Weight-bearing joints are sometimes affected more commonly than non-weight-bearing joints. Some forms of arthritis can also affect other parts of the body.
Juvenile arthritis is medically defined as continuous (also known as chronic) inflammation of one or more joints lasting at least six weeks, for which no other cause can be found in a child aged 16 or younger.
What causes Juvenile Arthritis?
No one knows exactly what causes JA. It is not caused by any disease or infection that either parent may have had. It is not connected to any event during pregnancy. JA is not caused by eating the wrong foods, and there is no proof that JA can be improved solely by any specific diets. Many people feel their arthritis is better in warm, dry climates, but there is no proof that JA is improved by any particular climate.
JA may begin after an event that switches on the body’s immune system, such as an ordinary infection or injury. The body’s immune system normally fights these infections or injuries by causing inflammation, which signals to the body to heal damaged tissue. However, the immune system should return to a non-inflammation resting state when the event has resolved. With JA, the immune system seems to become overactive and causes continuous inflammation. This continuous inflammation affects the joints and sometimes skin and internal organs.
Most types of JA are not passed from generation to generation so the chance of your child passing arthritis on to their own child is extremely rare.
How is Juvenile Arthritis diagnosed?
Children with arthritis do not always complain of pain, so it may be difficult to tell if a child’s joints are inflamed (red, swollen and warm to the touch). Sometimes the only initial clues to arthritis may be that the child is stiff when waking up or there is some difficulty using an arm or leg. In some cases, there may be no signs other than a swollen joint or some loss of movement. As a result, JA can be difficult to detect and may go unrecognized by even the most experienced doctor or healthcare provider. The child’s doctor will look carefully for any signs of joint swelling or loss of mobility, which indicate that the joints are inflamed.
Arthritis or its symptoms may be a result of many different illnesses, including infection, injury, allergic/drug reactions or other autoimmune diseases (such as thyroid disease, diabetes, inflammatory bowel disease or lupus). Since there is no single test to diagnose JA, tests to rule out other causes of joint pain and swelling must be done. Your child will likely have X-rays as well as urine and blood tests.
Once a diagnosis of JA has been confirmed, routine tests (such as blood tests, X-rays and eye examinations) will need to be repeated from time to time in order to follow the illness and assess the effects of any medication. Your child’s doctor will discuss with you how often these routine tests need to be done.
It is important to note that, depending on the type of arthritis, JA may be relatively mild or it an be progressive and disabling. The disease may be limited to the joints or affect the eyes and other organs. In some cases, with appropriate treatment JA can resolve by adulthood. With other cases, the disease and its effects are lifelong and require ongoing medical care.
The first several weeks following your child’s diagnosis can be a difficult time for everyone in your family. Your child’s condition may need to be reassessed in order for your child’s doctor to be absolutely certain of the diagnosis. It may take several weeks—or sometimes even months—for the medicines and prescribed therapy program to have a noticeable effect. If your child has started on medications or other treatments, the doctor will monitor these regularly.
What are the unique feature conditions
Growth. Inflammation from JA affects the growth of a child, meaning the growth patterns of affected joints may change. Sometimes inflammation can lead to quicker growth. However, growth usually returns to normal once the arthritis is under control. Sometimes if the inflammation is not well controlled, growth may slow down and ultimately not reach the full growth potential of the affected limb or digit. This makes controlling the arthritis to the point of no or minimal inflammation very important.
If the arthritis is severe and requires medications, such as steroids, overall body growth may slow down. Growth usually returns to normal once the arthritis is controlled and the use of steroids is reduced or stopped. The healthcare team will pay careful attention to all aspects of your child’s growth.
Eye problems and care. Many types of JA can involve inflammation inside the eye (called “uveitis”). This inflammation does not make the eye red, may not be painful and may not affect your child’s vision, so he or she may not even be aware of it. That is why it is important for your child’s eyes to be checked regularly by eye specialists. How often your child needs eye exams will depend on your child’s risk of developing eye problems and will be determined by your child’s healthcare team. If your child develops eye inflammation, then your child should be under the care of an eye specialist to receive appropriate treatment. Treatment may include eye drops, injections of steroids behind the eyes and other medications. Undetected or poorly treated eye disease can lead to vision loss or even blindness.
Eye disease can happen with any type of JA, and eye disease may begin before arthritis is even diagnosed. Eye disease is most common in children with inflammation in one or in only a few of their joints and having a positive marker in the blood known as antinuclear antibody (ANA). This antibody can be found in up to 25% of healthy children but can cause a higher risk of eye inflammation in children with arthritis. Testing for the ANA at diagnosis is important to decide how often your child will need to have a check up with an eye care expert.
Dental care. Arthritis of the jaw is seen in many children with all forms of JA. Your child may have no symptoms, or symptoms are felt as recurrent ear problems rather than arthritis of the jaw. If arthritis severely affects the jaw, the chin may not grow normally and rarely, surgery may be required. Parents/caregivers of children with JA should be aware of jaw problems, and they can occur at any time during their disease. If your child has trouble eating or complains about pain while eating, these symptoms should be reported to your doctor.
Treatment can include the usual rheumatology medications as well as local treatments such as mouth splints if recommended by an orthodontist. Because the metal in orthodontics braces interferes with MRI scans needed to monitor the jaw, please ask your orthodontist about ceramic braces. Different specialists are included in the care of children with arthritis of the jaw. Your child’s dentist should give your child’s teeth special attention and your child should practice good dental care.
Unpredictability. Rarely JA can be active for as little as several months up to a year, then it goes into remission and seems to “disappear” forever. Many children, however, have an up-and-down course for many years, depending on what type of arthritis they have. Flares are those times when the arthritis seems to be getting worse. Remissions are times when the arthritis seems to have disappeared. Sometimes a mild infection, such as the stomach flu, may cause a flare but the reason for a flare is usually unknown. Parents/caregivers may be upset to see a flare when it seemed the disease had disappeared or greatly improved. Yet parents should remain hopeful and optimistic because most flares will resolve with appropriate care and treatment.
What are the patterns and types?
The symptoms and nature of JA vary greatly. Once a doctor suspects JA, a child will usually be referred to a specialist, such as a paediatric rheumatologist (a doctor who is specially trained in the diagnosis, evaluation and treatment of joint, muscle and bone inflammation in children).
Anjolina Rankin-West is a Canadian Abilities Foundation (CAF) intern.