The value of pharmaceutical compounding:
An alternative method of pain relief and wound care
By Graham MacKenzie, B.Sc.(Chem), PhC, and John Ritter BA, MD, CCFP, DABEM
When was the last time you or a loved one took a medication and wished that it could have been fine-tuned—perhaps to have fewer side effects, or a more pleasant flavor, or another dosage form. Perhaps your home care patient has been prescribed a narcotic, but it caused nausea or constipation that prevented them from fully enjoying the pain relief it gave them, or even stopped them from taking it at all. Often gastrointestinal effects or an increase in blood pressure from NSAIDs are so profound, patients are unable to continue it. Maybe the off-label use of an antidepressant you took orally for pain resulted in such sedation or confusion, you were unable to even drive your kids to soccer or go to any social function. These effects are even more pronounced in the elderly population, who seem to present with side effects even when the dose is lower than that needed to treat the ailment.
Patients in nursing homes, hospitals or home care can have their quality of life reduced rather quickly with a painful pressure ulcer that can take a while to treat. Because of compounding, we now have individualized treatments for each patient based on how their ulcer presents itself.
The examples of patients who are helped by this type of individualized thinking are endless. The patient with external hemorrhoids who benefits from the compounded “rectal rocket” suppository that holds itself in position for both external and internal effect. The home care patient with the tissue ailment so painful that it cannot be touched, even when applying medicine to it. The chemo patient who needs extra local pain relief in the form of a tetracaine lollipop or dry mouth relief from pilocarpine in the same dosage form. The patient with chronic nausea who cannot keep down oral medications but responds to a topically applied mixture of the four medications. Compounding extends the quality of life for hospice, wound care and home care patients. It allows for the continuation of discontinued or short-supply medications, and pain relief for a myriad of conditions from migraine, plantar fasciitis, back pain, tennis elbow, shingles, carpal tunnel and more.
 Pain relief
Pain relief
The main goal of stopping pain with topically applied medications is to get to as many different receptors in the periphery as possible and block the transmission to the brain that registers as pain. Because of the wide variety of receptors involved, we are able to improve pain relief by targeting more than one receptor in a given topical. Some of these receptors are presynaptic (afferent fiber) or postsynaptic (in the dorsal horn cell in the spine). Because of the first-pass effect in orally administered drugs, doses need to be much higher than with topical medications, which go directly to the source of the pain.
Bases
Normal delivery bases such as Lipoderm® or PLO gel differ from other commonly used bases because our goal is to drive the active ingredient down across the stratum corneum into the epidermis and dermis. Lipoderm Activemax® is used when the total solute load goes over 20 per cent as the final product can become runny at this level.
Active ingredients
The success of pain relief is best dealt with in an approach that covers as many different receptors as possible in the periphery. Table 1 is a list of drugs, their typical percentages in the topical cream and the receptors they affect. Other ingredients such as magnesium chloride, amantadine, haloperidol, valproic acid, orphenadrine, tetracaine, glucosamine, chondroitin, MSM, piroxicam and others have all been used with success as well.
Application
These preparations are best applied six times daily, but we often have success with only one or two doses per day. They can be applied directly to the painful area but if a large area is affected (particularly in a limb), application to the source of the affected dermatome lateral to the spine on the affected side can cover the entire strip supplied by the nerve. Another commonly used method is to apply the medication to the trigger points of the muscle or muscle group causing the pain. This helps to cut down on the amount of medication applied and saves on wasting the cream.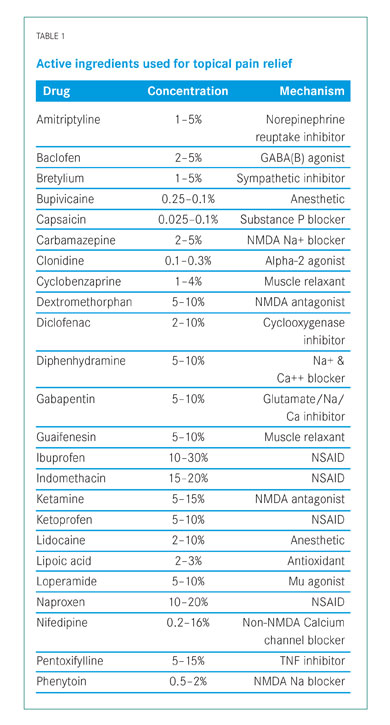
Wound care
Bases
Various bases are available that can be adapted to the type of wound. Polyox dressing has proven to be popular. This is a powdered base that can be mixed with powdered medications; it is applied with alternating sprays of water and allowed to set as a medicated shield. It has the ability to absorb several times its own weight in exudate from the wound. Even the water sprayed on the wound can have ketamine, lidocaine and other active ingredients dissolved in it.
A relatively new base, Occlusaderm®, a thermoactive gel, has shown promise in carrying medications; it turns from liquid to gel when taken from a refrigerated environment and applied to a body temperature wound. This is beneficial when there is a deep wound with crevices that cannot normally be reached with topical application. It can also be mixed with Lipoderm®.
Spirawash® is a base that is easily washed off a wound and holds active ingredients as well. It is good for wounds that need to be washed off on a regular basis with little force. It contains meadowsweet extract and has great healing properties for wounds, cuts, ulcers, burns and sores.
Pracasil® is another new base that helps healing and prevents scarring; it holds active ingredients as well. It contains pracaxi oil, an Amazon oil that has antioxidant, antibacterial and antifungal properties. It is an elegant anhydrous silicone base that works well in scar formulations.
Active ingredients
For infected wounds, a regular culture and sensitivity test can be done and the antibiotic can be included in the preparation. Metronidazole, clindamycin, aminoglycosides, vancomycin and rifampin are common examples.
Tissue regeneration is of prime importance in wound care. Infection and pain relief are necessary, of course, but the affected area needs to rebuild and repair itself for the ulcer to heal. One ingredient used for this is phenytoin. It has been observed that up to 15 per cent of patients on oral phenytoin experience gingival hyperplasia. This side effect is used in topical wound therapy, as it stimulates fibroblast proliferation, enhances tissue granulation, inhibits collagenase activity, promotes collagen deposition and decreases wound exudate production. This promotes wound healing.
Another commonly used ingredient is misoprostol, a drug commonly used in peptic ulcer treatment and prevention. It is a synthetic prostaglandin and has immuno-regulatory activity.
Calcium channel blockers such as nifedipine and diltiazem create vasodilation and white blood cell migration, and regulate prostaglandins. When applied to the wound margins, they are especially helpful in growing tissue back over the wound. Although the exact mechanism remains to be determined, it has been suggested that the drug-induced blocking of calcium influx into vascular smooth muscle may lead to reduced vascular tone,
which could increase nerve blood flow. Microvascular neogenesis and increased epithelialization are thought to occur through increased blood flow to the localized area of the pressure ulcer via this same smooth-muscle relaxation. It has been suggested that application of the nifedipine topically could theoretically lower blood pressure due to increased absorption of the drug. To date, this has not been documented. One side effect noted has been mild dry skin surrounding the wound. This is felt to be a sign of vasodilation and epidermolysis in the healed areas—a possiblesign that the drug is working.
Other ingredients used in wound care include tranexamic acid for bleeding wounds, and pentoxifylline, honey, sucralfate and cholestyramine for wound healing.
Application
Repeated daily application of dressings and compounds to wounds can be uncomfortable for the patient. When the wound is particularly sensitive, Spirawash® can be used as it easily washes off, although it may need to be applied more than once daily because of this property. Spraying with a lidocaine/ketamine aqueous solution before dressing application can be an added benefit as well. Polyox dressing is removed with slightly more shear force and may be applied once daily unless exudate is heavy. Occlusaderm® is also a dressing base that stays put when put into the wound because of its thermocactive properties. A cold cloth may help with removal of this base.
Dispensing containers
When accurate dosing of the final cream is required, quite often a device called a Topi-Click® dispenser is used. A metered pump dispenser is also helpful. These have the advantage of giving a consistent dose, especially when there are multiple caregivers (e.g., in hospitals). When the volume of each application is not crucial, the final cream may be placed in a plastic or metal tube that is sealed at the compounding lab. Polyox powdered dressing is dispensed in a collapsible puffer bottle that gives a fine stream of powder onto the moistened wound.
Physician and patient acceptance
One of the biggest hurdles to getting a patient to use these compounds is the comfort level of the doctor who will be writing the prescription. If this is the first time the doctor has prescribed these compounds, he or she will often prescribe just one ingredient or maybe two, and the dose will be quite low. Unfortunately, this often results in suboptimal results and a feeling of therapeutic failure, and the physician may drop the idea altogether. With so many receptors available, a “shotgun” approach is best so that many receptors are hit. In explaining this concept to the physician, I often compare it to many prescription treatments, like blood pressure meds, where maybe the first drug doesn’t work as well as first hoped. They increase the dose and maybe add a second drug that works by a different mechanism. Knowing how to write these prescriptions and follow up is important as well.
As far as patient acceptance of the creams, most will be open to whatever works, especially if it results in lower side effects. Acceptance by both parties is better when there are realistic expectations of the pharmacology of pain relief or wound care. Adjustments may be required. For example, opioids are normally not very effective for pain of a colic, muscle spasm or nerve destruction or deafferentation situation, and only partially effective for pain from bone, nerve compression or pleuritic origin. Visceral and soft tissue pain are best treated with opioids. The comfort level of both the patient and the health care provider is key as these preparations need to be applied properly for maximum benefit.
Case studies
93-year-old female Caucasian, cognitively intact. History of dizziness (chronic), recent diagnosis of anemia, compression fractures, increasing back pain. Pain meds include Endocet (with little relief), acetaminophen, and various OTC rubs (A535—not working—and Vick’s). Her pain sources were undetermined and her goal was to attend church without fidgeting or falling asleep. Prescribed diclofenac 6% and titrated ketamine up to 10% with lidocaine 2% in Lipoderm®. Goal was achieved with good pain relief.
74-year-old female Caucasian with synovial fluid collection in an area below the knee on the shin bone. Pain became focused in the foot due to pressure on nerve from the fluid pocket that developed. Somewhat relieved with acetaminophen, but pain worsened at night and bedtime when she would lie down. Applied ketoprofen 10%, ketamine 5%, clonidine 0.1% and lidocaine 3% in Lipoderm Activemax® when pain presented itself. Therapeutic goal to sleep pain free and not be bothered daily with pain. Patient reported complete pain relief when cream was used.
46-year-old Aboriginal male. History includes poorly controlled diabetes for 18 years; extensive chemotherapy for colorectal cancer and surgery with neurodegenerative disease. Impending renal insufficiency. Pain sources included diabetic neuropathy (moderate) and post-chemo neuropathy in extremities (severe). Pain goal was to walk without severe pain in feet. Applied ketamine 6%, gabapentin 6% (neuropathic pain) and lidocaine 2% in Lipoderm® base. Good pain relief achieved.
79-year-old male Caucasian, creatinine clearance 26. History includes remote upper GI bleed, thoracotomy for empyema, coronary artery disease and arthritis in the neck. Pain source was mixed post-thoracotomy pain and musculoskeletal pain. Pain goal was to sleep well and not wake up wife, and not upset wife by taking narcotics. Applied ketamine 10%, gabapentin 2%, ketoprofen 10% and menthol 0.5% (medicinal smell so the patient thinks it works, and actively acts against pain) in Lipoderm Activemax®. Patient reported goal reached.
References available on request.
Graham MacKenzie, B.Sc (chem),PhC, is pharmacist/owner as well as chief compounder and nutraceutical advisor at Stone’s Pharmasave in Baddeck, Nova Scotia. He can be reached at graham@stonespharmasave.com or 902-295-2404.
John Ritter BA, MD, CCFP, DABEM is a palliative care physician covering much of Cape Breton Island, Nova Scotia. He embraces compounding practices in his regular prescribing.