By Dr. Isabelle Vede and Dr. Saskia Sivananthan
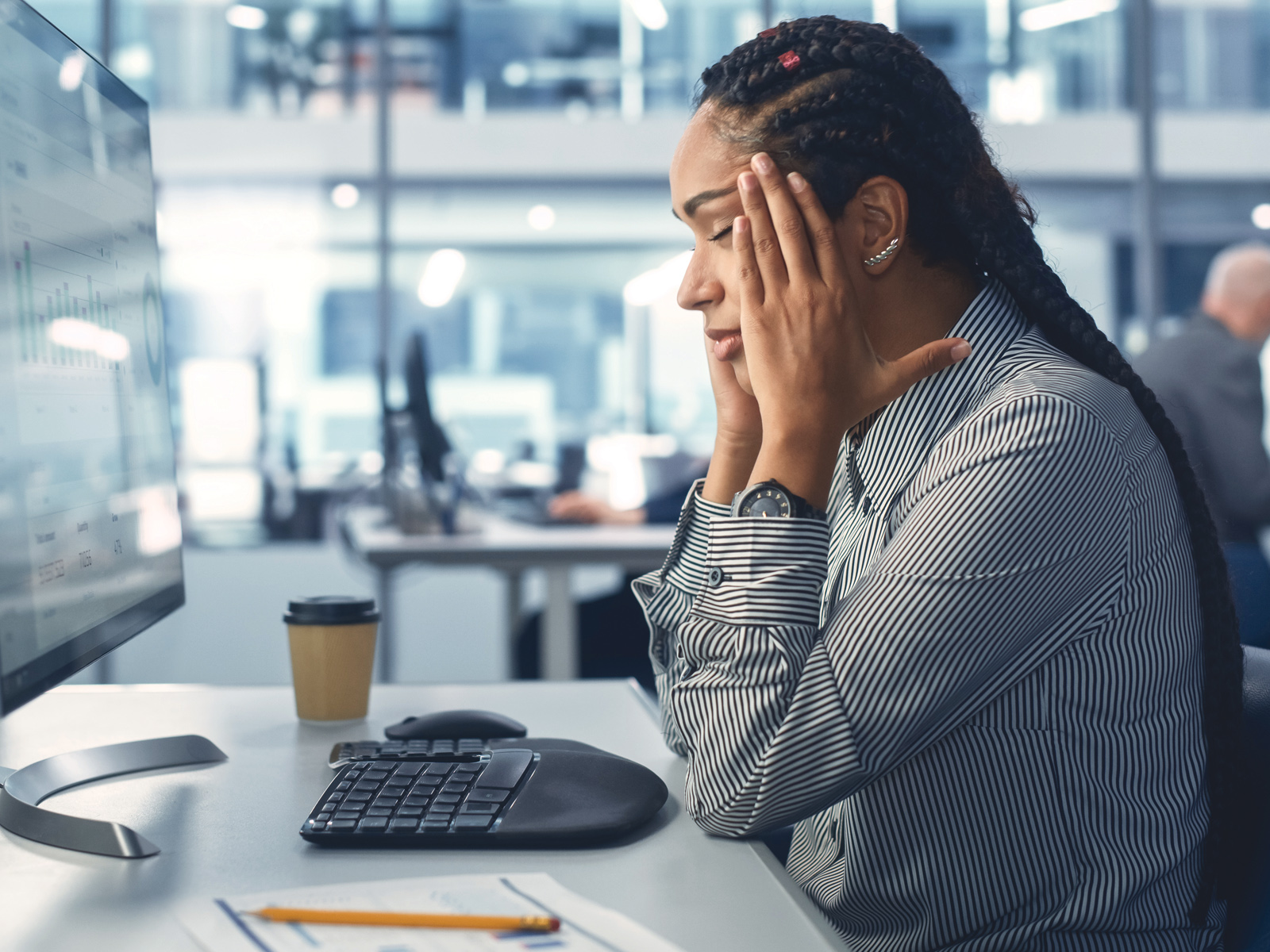
The COVID-19 pandemic has forced most of us to adapt to new daily routines and navigate new ways of handling everything from regular errands to safe socializing and work. It has been a stressful and strange time, to say the least, but it has been especially difficult for older adults living with dementia.
“People living with dementia have been heavily impacted by the pandemic,” says Dr. Isabelle Vedel, a public health physician and professor in the Department of Family Medicine at McGill University. “Not only are they at increased risk for severe illness and death from COVID-19, they are also particularly vulnerable to consequences that go beyond the risk of infection. For example, the sudden loss of social contact and stimulation [because of the need for physical distancing and service/program closures] can increase isolation, anxiety, and depression, which ultimately leads to poorer health. And for caregivers, there’s the added stress of essentially being left alone to provide care at home or of not being able to visit their loved one in a long-term care facility. It’s a very difficult situation.”
The Alzheimer Society of Canada knows first-hand the huge stress and negative impact the pandemic has had. “We have daily, heartbreaking calls from clients who are at the end of their rope, who are living in the community and have had all forms of support cut off, no respite, are struggling to contact their doctor or are too scared to bring in support because of the real fear of contracting COVID-19—or worse, having the person they love, who is already living with dementia, develop COVID-19,” explains Dr. Saskia Sivananthan, Chief Research and Knowledge, Translation & Exchange Officer from the Alzheimer Society of Canada. “And we are equally concerned about whether people living with dementia are not going to the emergency department, putting off surgeries and ignoring other symptoms because they are afraid of accessing the health system during the pandemic. But we don’t have adequate data to help us understand if this is the case, and what the consequences are.”
To address this need, Dr. Vedel is now leading a study to measure and describe the real-life pandemic experiences of people living with dementia and their caregivers, including for those living in a community setting or in long-term care. This information will ultimately help the team develop evidence-based strategies and recommendations for policy makers, health system managers, clinicians, and community organizations to reduce the impact of unintended harms stemming from public health measures and to help people living with dementia stay safe and healthy throughout the pandemic.
Gathering this information is an enormous undertaking, but Dr. Vedel has been able to pull the project together quickly by working with the Alzheimer Society of Canada’s COVID-19 and Dementia Task Force and leveraging her existing relationships with fellow researchers through the Canadian Consortium on Neurodegeneration in Aging (CCNA). The research project itself consists of several parts. To measure the impact of the pandemic in terms of health and social services use, as well as mortality rates for people living with dementia, the team will analyze data from provincial databases about hospital admissions, visits to the doctor, and homecare services. With this information in hand—which can take anywhere from three weeks to five months to gather, depending on the province and the associated data access protocols—the team will interview people living with dementia and their caregivers to get a better sense of how they have managed throughout the pandemic.
“We want to learn more about their experiences and how they have been living,” says Dr. Vedel. “Are their needs being met? They may have been able to get a virtual appointment with a physician, for example, but those virtual visits can be challenging for people with cognitive issues—so has it been enough? Have they otherwise changed their approach to care? And for those living in long-term care, where up to 80% of residents have some sort of cognitive impairment, we can calculate the infection rate—but how are they coping? The provincial data will give us the numbers, but these interviews will show us real life.”
For Dr. Sivananthan and the Alzheimer Society, focusing on these lived experiences is second nature. “We do not embark on any major initiative without working in direct consultation with people living with dementia and their caregivers,” she explains. “Their early active and meaningful engagement is crucial in making key decisions about the direction and impact of the work we intend to do. As researchers, policy makers, and decision makers, we understand how to collect and interpret the evidence, but this is a bit like looking at things in black and white. Engaging people with that lived experience puts the evidence in context—like making things technicolour.”
With the support of Dr. Sivananthan and the Alzheimer Society of Canada, Dr. Vedel’s project team includes people living with dementia and caregivers, who will help shape the interview questions and discuss the results. The team also plans to host consultations with policy and health care stakeholders in early 2021, with the ultimate goal of having the final policy recommendations and strategies available in the spring. In the meantime, the team will release meaningful updates through newsletters, social media, and webinars to support improvements along the way.
“We can make things better,” says Dr. Vedel. “In fact, we have to.”
This article was reposted with permission from Canadian Institutes of Health Research. Visit cihr-irsc.gc.ca/e/51981 for more research on COVID-19.