By Cathy Choi
Bariatric clients often have comorbidities that cause added complexity for prescribing therapists.
In the current health care climate, therapists may find themselves with little time to complete assessments for wheelchairs and under pressure to be efficient. Simultaneously, because of the rising prevalence of morbid obesity, 1referrals for bariatric power wheelchairs are on the rise.2 Bariatric power wheelchair assessment and prescription, however, is complex and requires a thorough and individualized process.3 Bariatric clients often have comorbidities, which can include any diagnosis that practitioners encounter with other seating and mobility clients, and also medical complications from obesity.4 Therefore, there are several complexities regarding the seating and mobility needs of bariatric clients, unique to this population, that must be considered.
With all this in mind, therapists may feel uncertain about assessing and prescribing power mobility for bariatric clients. The purpose of this article is to provide therapists with a guide of factors to consider when assessing and prescribing bariatric power wheelchairs.
Some unique complexities
Morbid obesity is highly linked to lower-extremity edema, chronic venous insufficiency and lymphedema.5 In lymphedema, lymph fluid does not drain appropriately, accumulates and leads to swelling.6 This swelling can be quite pronounced in bariatric clients, and can interfere with mobility and positioning for engagement in daily activities.
Extra adipose tissue also affects positioning and the ability to provide appropriate support to the skeletal posture underneath the adipose tissue. During seating assessments, excess adipose tissue can also create a challenge when it comes to landmarking key areas that are typically used to take accurate measurements. The client’s tissue distribution and the effects of gravity also impact posture and supportive positioning needs.
Lastly, skin integrity must also be considered when prescribing seating surfaces and positioning changes. Skin breakdown can occur in the skin folds of the abdomen, groin and popliteal fossae. Skin breakdown also occurs from shearing forces when transferring onto and off seat surfaces, and from pressure injuries caused by immobility and a poor ability to weight-shift. In view of these multiple unique factors, a thorough and individualized assessment process is required for bariatric clients.
Assessment guide
The following assessment recommendations are based upon clinical experience derived from collaborating with bariatric clients in order to understand the challenges they experience with their power wheelchairs.
1) Home and community environments
A customized power wheelchair may end up fitting the client beautifully, but if it does not also fit the client’s environment then it is essentially useless.
• Environmental factors to consider in the home are doorway widths and the space available in the home layout to complete turns with the power wheelchair. Therefore, knowledge of the overall width of the wheelchair and its turning radius are essential in ensuring the wheelchair will fit in the client’s home.
• Ramps will be needed to gain entry/exit, and they must be built to comply with building codes.
• The outdoor terrain in the client’s neighbourhood is also an important factor, as the terrain the client must traverse on a regular basis can affect the drivability of the power wheelchair and the client’s safety. Are the sidewalks in good condition, or are there many potholes and cracks? Are there appropriate curb cuts or are they too steep? Are there abrupt transitions from the sidewalk to the road? Are there many hills?
• The client’s centre of gravity is another factor. If the client is placed too far forward over the base of the power wheelchair then the front casters become overloaded, reducing drivability—especially on sloped and uneven terrain. A forward centre of gravity can also lead to forward tipping of the power wheelchair on downward slopes, steep curb cuts and at abrupt transitions in paved surfaces such as cracks and potholes.
Bariatric clients can sustain severe injuries from tipping forward out of their wheelchairs. Therefore, it is strongly recommended that the client trials the power chair at home and in their neighbourhood while accompanied, before deciding on a model and making a final purchase.
2) Taking measurements
Measurement surface. Making a home visit can provide valuable context. A home-visiting therapist will need to be resourceful when measuring bariatric clients. First and foremost, measurements of the client should not be taken while the client is lying supine on a bed or sofa. Measurements in supine will essentially be inaccurate, as the client’s tissues will rest very differently when lying as compared with sitting, which is the target posture. Moreover, the critical measurement of seat depth does not exist in supine lying, as seat depth simply cannot be equated with thigh length in the bariatric client. Inaccurate measurements will lead to an inaccurate wheelchair prescription, which can be extremely time consuming to correct and can result in inadequate postural support and pressure injuries.
Measurements are best taken with the client in a seated position on a firm and flat surface, with the feet well supported. To achieve this, therapists might need to request joint visits with other health professionals to help with transfers and positioning. If a plinth is not available, then a large transfer board or rigidizer can be placed underneath the client while the client is seated on a bed or sofa to help achieve a firm and flat surface. If the surface is not firm and flat, then the client will exhibit postural leaning and hip adduction and internal rotation, resulting in inaccurate measurements.
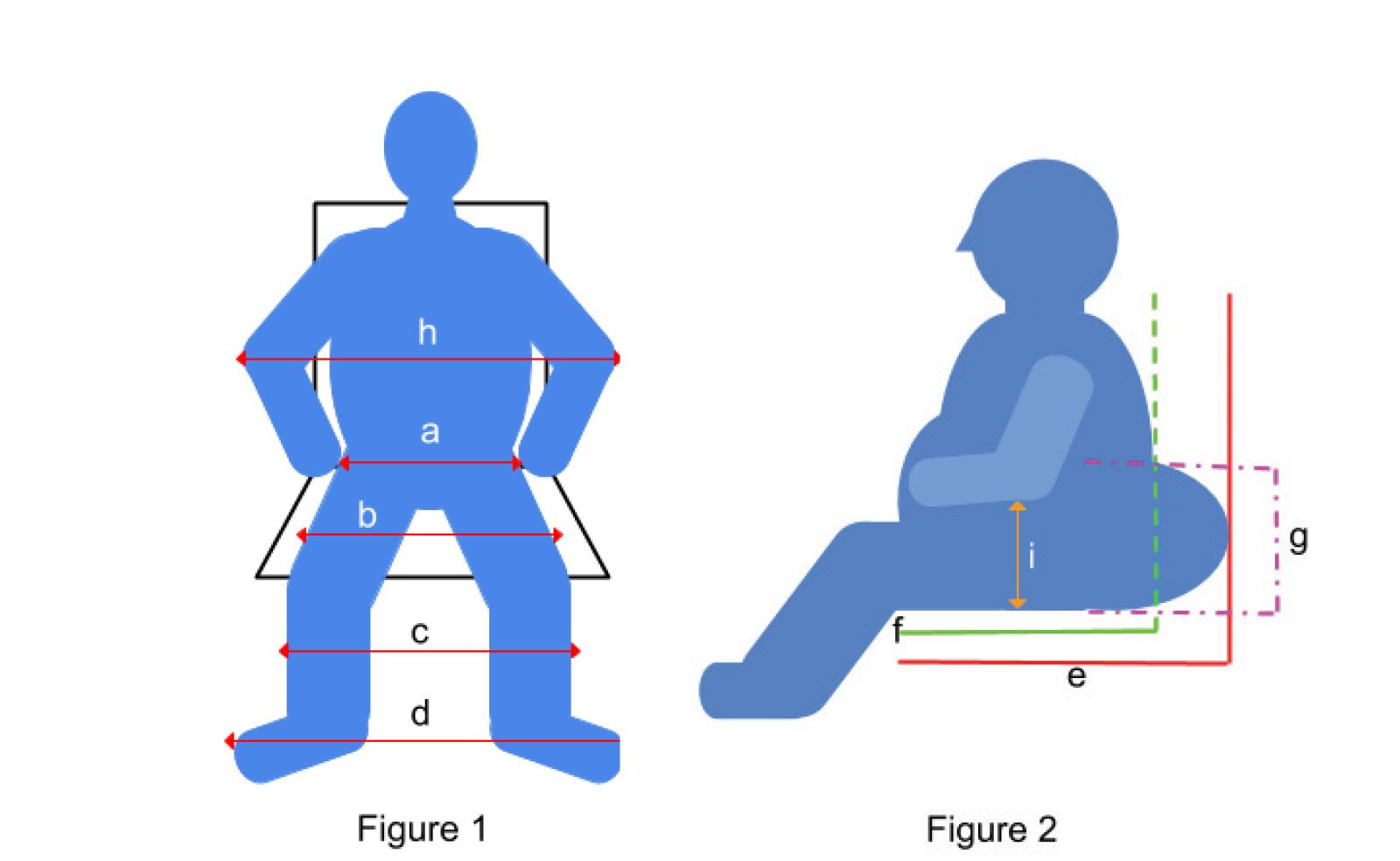
Key measurements. With bariatric clients, additional measurements must be taken to ensure appropriate prescription (see Figures 1 and 2).
•Hip width across the pelvis (a) can be measured using calipers.
• Due to edema and adipose tissue, however, seat width measurement should also take into consideration the overall thigh width (b).
•The width across both lower legs (c) is important, as edema and adipose tissue may result in the lower extremities impinging on leg rests and hardware.
• The width across the feet (d) is also needed to ensure proper foot placement; the feet of bariatric clients may need to sit farther apart. When forced closer together on a footplate that is too narrow, pressure can increase at the lateral aspects of the feet, as the client’s hips abduct and externally rotate and the feet supinate to help keep the feet on the footplate.
• Two measurements are needed for depth: The seat-pan depth from the popliteal fossa to the posterior of the buttocks (e), and the actual seat depth from the popliteal fossa to the posterior trunk (f).
• The actual seat depth (f) and the height of the gluteal shelf (g) directly impact backrest placement. The backrest should accommodate the height of the gluteal shelf and not be placed at seat-pan depth (e), as in this position the backrest will not contact the client’s actual trunk, unless the client leans back into lordosis or slides into a posterior pelvic tilt.
• Lastly, for appropriate arm support, the width across the elbows (h) and the forearm height with the elbows flexed (i) are needed. Without adequate arm support, clients may experience shoulder girdle pain from the downward pull of the weight of their arms.

3) Power positioning and electronics
Power positioning functions can be highly beneficial to bariatric clients. Power leg-rest elevation enables repositioning of the legs, helps manage skinfold breakdown in the popliteal fossae, alleviates pressure at the feet and, when used in conjunction with power tilt, helps facilitate circulation and manage edema in the lower extremities.7 Tilt assists in shifting the client’s centre of gravity rearward over the wheelbase, reducing the feeling of tipping forward when driving down slopes. Tilting also enables clients to weight-shift when sitting, providing pressure relief at the ischial tuberosities when tilted past 25 degrees.8 Anterior tilt, which brings the front of the seat pan lower than the rear of the seat pan, can improve transfer biomechanics and reduce shearing forces on the client’s seated surface when transferring. Recline increases the seat-to-back angle and can help relieve pressure from the weight of the abdomen resting on the thighs, manage skinfold breakdown at the groin and, when used together with tilt, reduce pressure at the ischial tuberosities.
Of final consideration are upgraded electronics and autocorrection systems. Therapists may consider these functions useful for clients predominantly with upper-extremity weakness and neurological conditions. Upgraded electronics functions can also help to improve the responsivity of the power wheelchair as it drives over uneven terrain while carrying bariatric weight.
When prescribed appropriately, power wheelchairs can greatly improve the daily function and safe mobility of clients. Because bariatric clients have unique medical and functional needs, care must be taken to ensure that both the client and their environments are thoroughly assessed
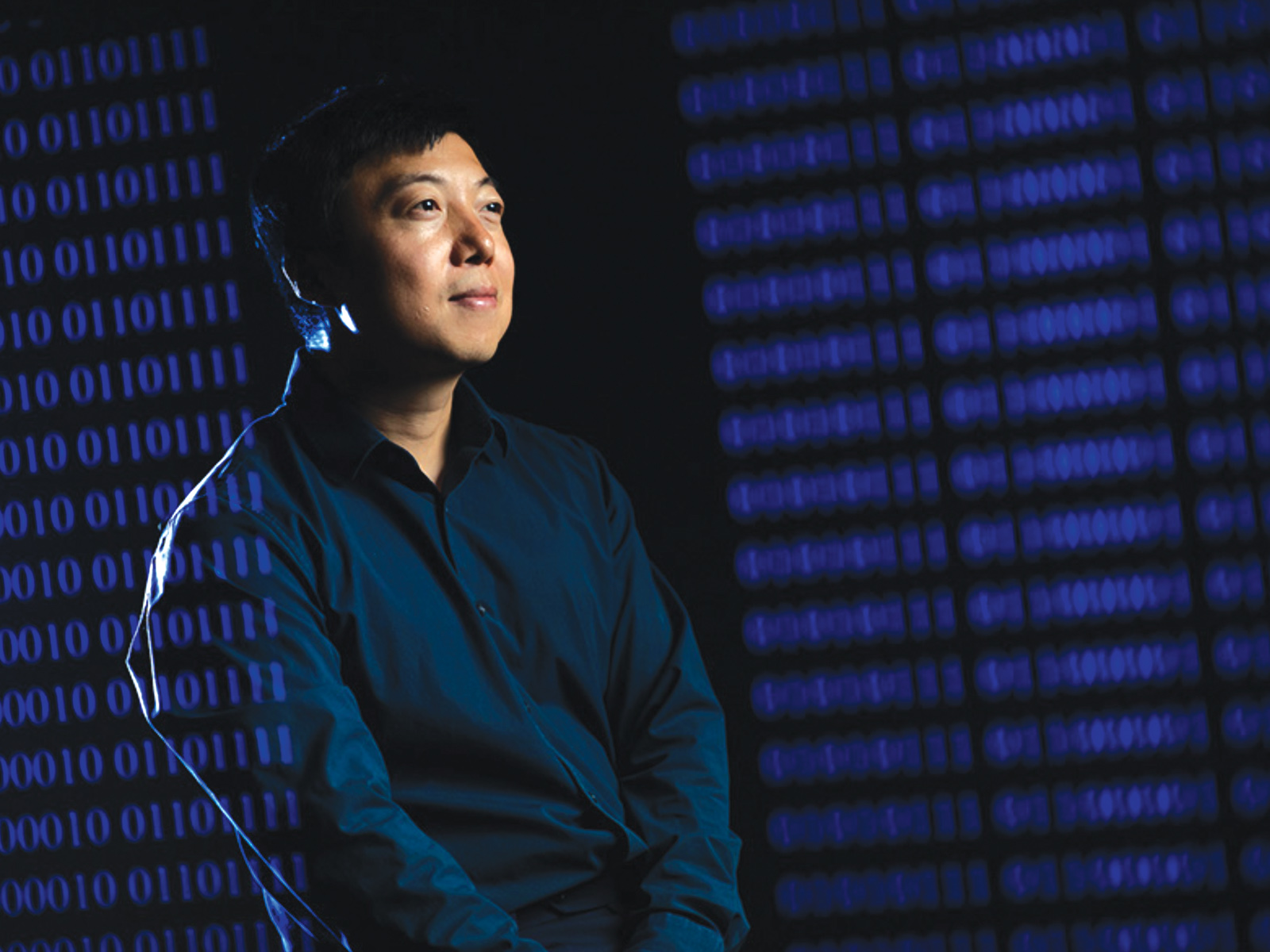
Cathy Choi is an occupational therapist who is passionate about working with adults in complex seating and mobility. She works at Sinai Health System, Bridgepoint Health Active Healthcare Seating Clinic in Toronto.
References available on request.