While dying is a normal passage of life, death is often treated as an illness. As a consequence, many people often die alone in hospitals and, unfortunately, in pain.
By Anthony Milonas
For many seriously ill patients, hospice palliative care offers more dignified options in the last days, weeks or months of life by providing a comfortable alternative to spending the period at end of life in a sterile, if not impersonal, environment. It neither hastens or postpones dying, but rather its end goal is patient comfort surrounded by family in a setting of their choosing—whether in assisted living, residential care or in the community—and experience a natural, more comfortable death.
A look at funding
The challenge is in the lack of funding specific to palliative care. For patients, they do not get the care they want, or what they need: 74 per cent of Canadians have thought about end-of-life, but not all Canadians who die currently have access to, or receive hospice palliative and end-of-life care services. Also of note is the fact that 93 per cent of Canadians believe hospice palliative care should be provided in the patient’s setting of choice.
For funders, this is much like a domino effect: yes, people prefer to die at home if given the choice, but because of the lack of access, most will likely have to die in a hospital setting. This then boosts associated overall costs.
 Take the province of Ontario as an example: According to Home Care Ontario, caring for terminally-ill patients in an acute-care hospital is estimated to cost over 40% more than providing care in a hospital-based palliative care unit, more than double the cost of providing care in a hospice bed, and over 10 times more than providing at-home care.
Take the province of Ontario as an example: According to Home Care Ontario, caring for terminally-ill patients in an acute-care hospital is estimated to cost over 40% more than providing care in a hospital-based palliative care unit, more than double the cost of providing care in a hospice bed, and over 10 times more than providing at-home care.
Home care is not considered an essential service guaranteed by the Canada Health Act; rather, it is provided on a regional and local level, with funding from provincial and territorial levels of government. “We know that introducing a broad range of palliative services earlier to people who are very ill, aging, or frail improves quality of life for people to live well until they die. But, it also costs far less than the acute care option,” says Sharon Baxter, Executive Director of the Canadian Hospice Palliative Care Association. “But most Canadians don’t have access to—or even awareness of—the full spectrum of palliative care services, especially those that deliver at a high level of clinical excellence.
Given we are all living longer, often with chronic illness, this awareness level and access to care need to change.”
The Government of Canada is committed to helping ensure that Canadians receive the compassionate care they need by providing $3 million over three years to the Pallium Foundation of Canada to support training in palliative care to front line health care providers. As a result, the need is expected to increase as the public becomes more aware of its benefits.
These demands on the healthcare system require consideration of new care models to improve coordination, continuity, access, and quality of care, and it is imperative that an interdisciplinary palliative care team is instituted to provide a combination of services, ranging from nursing to social services and physician care.
LEAP — a family-centred approach
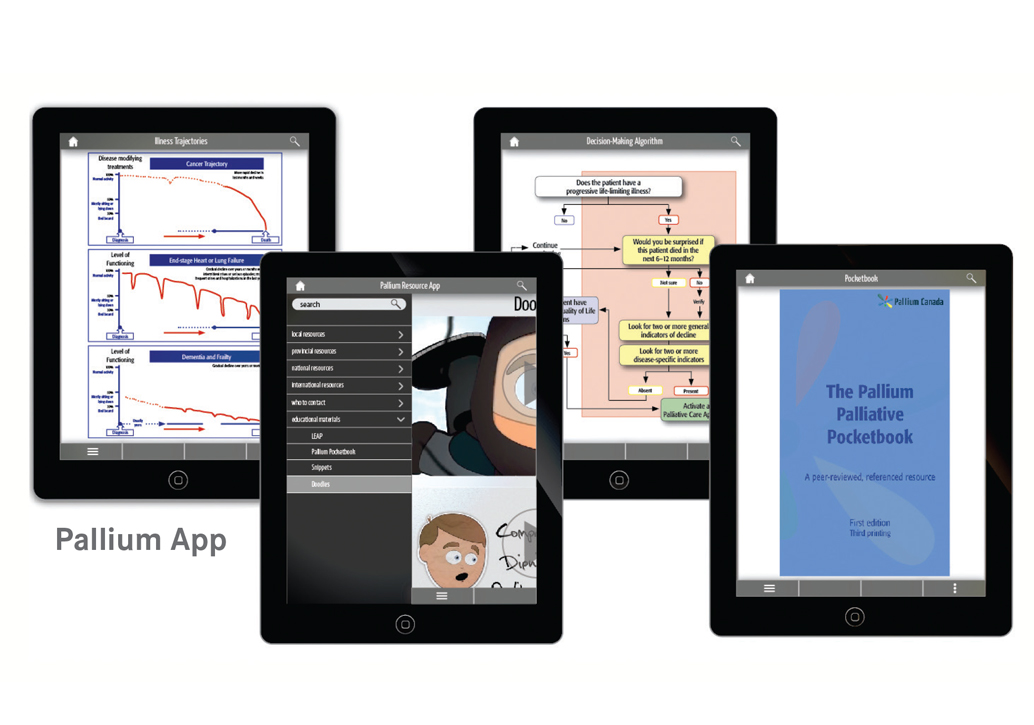
Helping to standardize care, LEAP (Learning Essential Approaches to Palliative and End of Life Care) is a competency-based approach to enhancing palliative care services across Canada for patients with life-threatening and life-limiting illnesses.
Developed by the Pallium Project, it operates as an agent for change on family practice and community settings to bolster inter-professional collaboration and support both for individual and team practice. “It’s a person-and-family-centered approach to patient care so that patients and families may benefit from the full scope of experience and competencies of various disciplines,” says Rosanna Dolinki, a Registered Nurse and National Senior Manager of Clinical Practice at CBI Health Group. For Dolinki’s teams that provide palliative care, having this education proves a level of clinical excellence and gives their health care providers an opportunity to connect with the resources and other palliative expertise in their local area. This makes transitions of care more seamless and reduces possible risk, she says.
Developed by content experts across Canada, the inter-professional program uses practical and case-based studies for a multi-disciplinary group of healthcare professionals, like: nurses, physicians, social workers and family caregivers. Given the fact that a palliative patient’s needs are expansive and not just needed in that specific moment of time of that person’s death, it is critical to build this continuum of care with an interdisciplinary mindset. Access to treatment must be consistent, and this support team will ensure it is fair to all who need it.
Competency across the illness trajectory
Competencies are developed on the growing evidence supporting an integrated palliative approach to providing care. Based on the Canadian Hospice Palliative Care Association (CHPCA) Model to Guide Hospice Palliative Care, it emphasizes palliative care across the illness trajectory, from the time of diagnosis of a life threatening, life limiting illness to the terminal phase (“end of life”) and beyond to grief and bereavement care.
Courses run the full spectrum so health leaders responsible for quality improvement can strive for the best care possible. Some examples of modules include: decision-making, grief, nutrition, psychological and spiritual care, advance care planning and essential conversations. It is aimed at health professional teams who are committed to providing quality care, especially pain and symptom management, in the context of collaborative, community and clinic-based settings.
“As an industry leader, having a national, integrated network increases our opportunity for learning and sharing skills,” Dolinki states. “This education program ensures consistency that we are providing the most up-to-date best practices across the country.
Anthony Milonas is Chief Operating Officer at CBI Health Group, where they offer an integrated approach to connect the dots for palliative care service.













