Deprescribing: A Popular New Team Sport in Rehabilitation
By Dr. Cara Tannenbaum
Polypharmacy is emerging as a silent epidemic among seniors. “Poly” means “many” and “pharmacy” refers to medications. The data are alarming: Two out of three seniors aged 65 years or older are prescribed at least five different medications. More than a quarter take at least 10 medications each day. Forty per cent of seniors older than age 85 years are prescribed at least 10 different medications. Older women are most at risk. The good news is that it is never too late to re-evaluate one’s pills, or those of a patient or loved one. A stay in a rehabilitation facility and periods in which home care are necessary are perfect opportunities to take stock of which pills are still needed, and which can be discontinued or “deprescribed.” Sound familiar?
Older adults are more at risk for med side effects
Reasons why aging increases the risk of harmful med side effects:
• the brain becomes more sensitive to drug effects
• medications stay longer in the body because of less muscle and more fat
• the liver and kidneys process medications less efficiently
• medications can become more concentrated because of less body water
Sometimes, medication side effects are not correctly identified as such. This leads to an additional medication being prescribed to treat the symptoms caused by a medication the senior was already taking—a phenomenon known as a “prescription cascade.” A prescription cascade can cause a patient to be prescribed multiple medications, which may be unnecessary or even harmful. One example is constipation caused by an antihistamine or codeine, which is what happened to Martha. Laxatives and sometimes enemas are then prescribed to treat the constipation.
Taking a number of medications increases the risk of drug interactions. Seniors taking 8 to 10 medications have an eight times greater risk of drug interactions than a patient who takes 2 to 4 medications.

Which meds are riskier than others?
Not only are seniors at higher risk of harmful effects of medications and interactions than younger people but, sadly, data indicate that 40 per cent of seniors take potentially inappropriate medications. A medication is considered inappropriate when the risks outweigh the benefits and safer alternatives exist.
In short, seniors are the victims of an overprescribing epidemic. Their heightened sensitivity to harmful effects and their vulnerability to drug interactions, combined with the use of potentially harmful drugs, has serious potential consequences: Falls,
fractures, memory problems, hospitalization or even death.
Let us start deprescribing
“Deprescribing” is the process of stopping or reducing the dose of a medication that might no longer be of benefit or may be causing harm. The goal of deprescribing is to maintain or improve the individual’s quality of life.
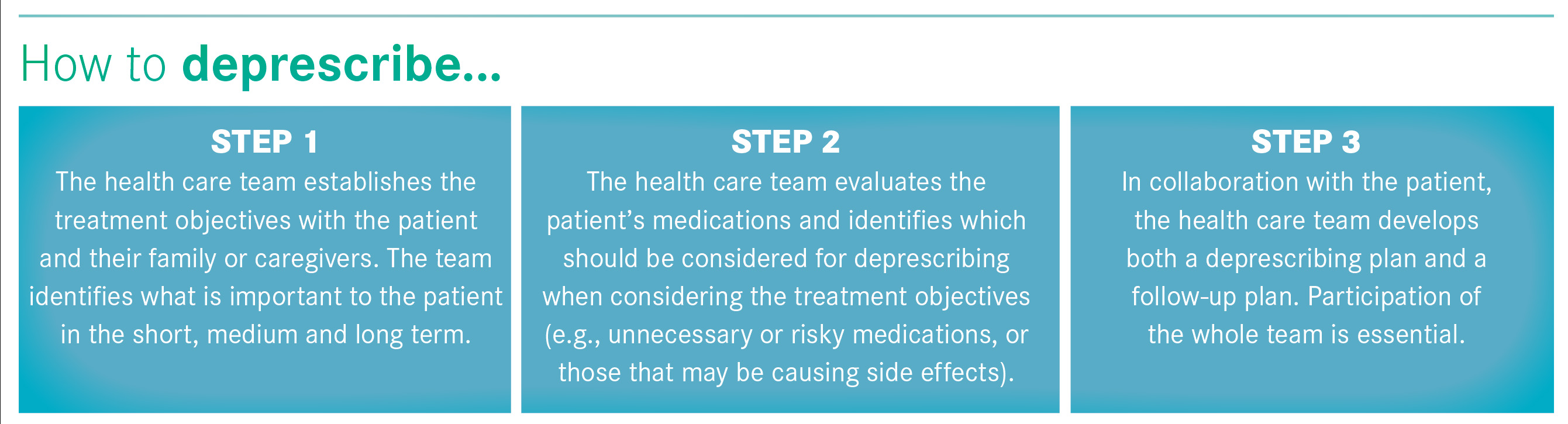
Deprescribing is a team effort
The entire health care team has a role to play in deprescribing to prevent cases such as those of Martha and Frank—it is not just
the physician’s responsibility.
Here is an example of how the entire interdisciplinary health care team can help to deprescribe a sleeping pill in order to reduce memory impairment, daytime sleepiness and the risk of falls and fractures.
• Nurse—monitor the impact of medication changes, and provide education and support by implementing non-pharmacologic approaches (e.g. cognitive behavioural therapy for insomnia).
• Pharmacist—develop a tapering schedule for the sleeping pill, monitor the patient and adapt the tapering schedule as needed.
• Beneficiary attendant—help evaluate the impact of medication changes throughout the tapering process and alert the team to problems, if required.
• Social worker or psychologist—help implement non-pharmacological strategies during deprescribing. For example, managing anxiety and depression can help treat insomnia.
• Physiotherapist/kinesiologist—help develop an exercise/stretching plan to reduce pain (where appropriate) and improve activity levels during the day.
• Occupational therapist—help develop individualized sleep routines and limit barriers to sleep (e.g., light, noise).
• Dietician—ensure a proper diet and eliminate caffeinated beverages at suppertime, which can negatively impact sleep.
• Administrator—establish appropriate resources and structures to allow deprescribing.
In the next edition of Rehab & Community Care Medicine, I will discuss identifying and targeting medications for deprescribing. These medications can undermine a patient’s rehabilitation process and put them at risk of harmful effects. To learn more about deprescribing, visit deprescribingnetwork.ca.
References available upon request.
Dr. Cara Tannenbaum is co-director of the Canadian Deprescribing Network and Professor of Medicine and Pharmacy at Université de Montréal.