By Jen St. Denis and Moira Wyton
British Columbia lost more people to toxic drugs in 2021 than ever before. At least 2,224 people died. Every month or two, the government says it’s moving as quickly as it can but frontline workers staffing overdose prevention sites, doing outreach in encampments, reversing overdoses and connecting people with safe supplies of substances, treatment or recovery services, say that’s not happening.
Here, six frontline harm reduction workers tell us about how the toxic drug crisis is playing out across the province.
Danielle Kennedy: HIV/HCV outreach educator, AVI Health & Community Services, Campbell River
I came back to work after my maternity leave and found my funding was cut.
A lot of people live rough, and without our overdose prevention room funding, we have nowhere near the inbound foot traffic. People aren’t coming in so we can’t find them and we haven’t been given tools to bring people in.
People are dying left, right and centre. And nothing’s changing. And, there’s been a big change of drugs. Benzos (benzodiazepines) a class of anti depressants are pretty brutal when added without the user knowing. It’s still an OD but requires a lot more attention. I’ve monitored someone for three hours, alone in the field. Plus, we only have two oxygen tanks and one oximeter right now.
The treatment centres here in Campbell River don’t work. We need more – things like second-stage and long-term housing and a SAFER [Safer Alternatives for Emergency Response] program like they have in Victoria for safe supply,
Jon Braithwaite: Board member and supervisor, Vancouver Area Network of Drug Users, Vancouver
Over the past year, the benzos started to get mixed in with the fentanyl. At first the dealers were putting fentanyl into heroin causing a wave of deaths. Then, dealers started putting benzos into dope. After a hit it was lights out for hours or even days. I’ve met three girls now that have been raped because of it.
It’s like a war out here. Every day you hear of somebody either OD’ing, or violence that happens because of the drug trade. When someone starts out, they’ll talk a good game and the dealer will say, ‘OK, well I’ll give you a zip of this’ — a zip is an ounce—‘and I’ll give you a week to move it. At the end of the week if they don’t have the money violence comes into play.
Juls Budau: Master’s of social work candidate, freelance writer and research coordinator, Prince George
I’ve worked a lot of roles in the overdose crisis the past year: in harm reduction housing, overdose prevention, as a substance use support clinician, and now I’m writing my thesis for my master’s in social work, which is looking at user perspectives
on stimulant safe supply and what it means to the users.
More people die of overdoses every month, but the provincial government keeps bragging about what they are doing so the public perception is that we’ve done everything we can and it’s not working. But service gaps haven’t been filled. There aren’t places for people to safely consume drugs in communities or and safer prescription alternatives and safe. There are misconceptions about what medical safe supply is and no evidence that it’s contributing to deaths.
Many of my clients use both meth and safer prescription alternatives, but the methadone prescription is cancelled if they miss a few days. Then they have to seek out a new prescription—not available every day in Prince George. The result: This instability leads to more chaos in their lives.
Garry Sandhu: Peer coordinator and addictions counsellor, Sober Life Foundation, Surrey
When COVID started we set up a phone like to be connected with people in addiction. During the last year, we received around 350 calls. [The One Life Peer Support Line can be reached at 778-381-5686.] I was in addiction and looking for help in 2012. I couldn’t find resources in Punjabi or Hindi and couldn’t express my emotions and feelings—very important if you want to be in recovery and come out of addiction. So, when I became sober, someone suggested to me that I go to school to become an addiction counsellor.
In our culture, mostly families get connected first, before a person calls for help for himself so when I finished my studies, I wanted to create a program especially for the Punjabi community.
We knew that when the COVID-19 restrictions started, addiction numbers would go higher and there would be mental health issues. But, we did not expect street drugs to become so much more harmful. We used to discuss complete abstinence as well as harm reduction, but because of the dangerous drugs on the streets, we promoted harm reduction more in order to keep people safe from the street drugs. In complete abstinence, if someone relapses, there is a huge chance he could overdose. If a person is on a harm reduction program taking methadone or suboxone, at least he will be way safer.
Trey Helten: Manager, Overdose Prevention Society, Vancouver
It seems like there’s just less and less people. Alleyways are less crowded, and numbers are going down. People aren’t moving on, getting healthier, planning safe supply options or going to treatment. They’re all dead. There’s no other way to put it. It’s just, funerals, funerals, and funerals because of tainted supply.
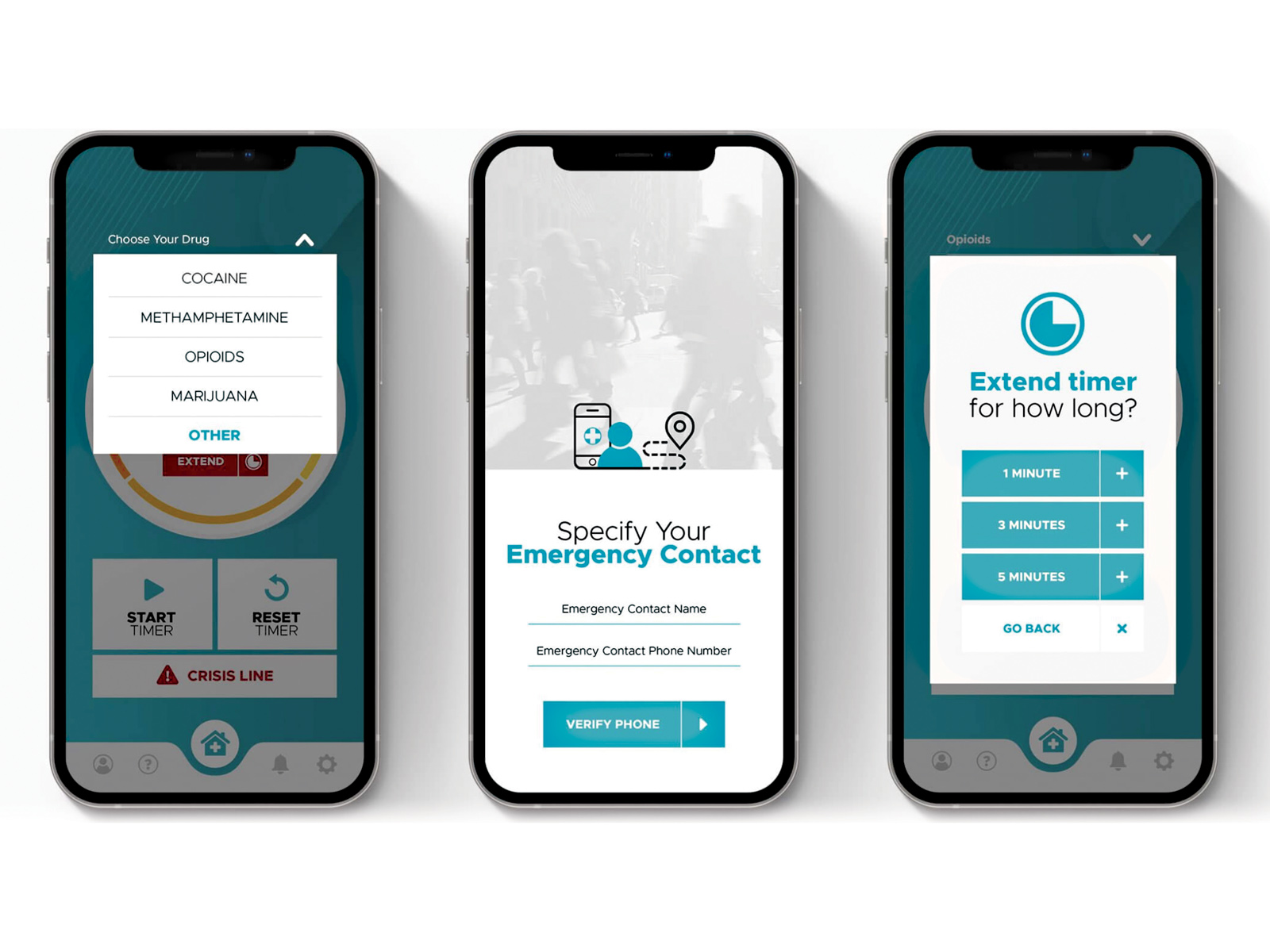
I encourage people not to use alone or use the Lifeguard app or the Brave app to tell us they’re about to use, what substance that they’re using and their location. They click the start button once they’re using. If they don’t check in… we can send paramedics.
Alexis Hekker: Indigenous wellness coordinator and lead drug-checker, ANKORS East Kootenay, Cranbrook
Most of the people we lost in our community in the last few years have been Indigenous. In 2019, harm reduction was actually working and we had so much hope.
And then, deaths just piled and piled and hit like a brick wall in 2020. Many of them were Indigenous women at risk and living rough. If you’re Indigenous, you’re over five times more likely to die of any kind of fatal drug poisoning.
What I needed was connection to my community as Métis person and citizen of the Métis Nation BC. That can sometimes be very hard. If I have a little bit of money to buy somebody a meal that is traditional, some fried bread and some bison stew, I will. I’m teaching other people how to bead because that was a huge turning point for me when I was able to learn how, and why that was so important to my culture. I’m now renting an office at Operation Street Angel, which is run by the Ktunaxa Nation and trying to decolonize harm reduction in a way, but I’m learning as I go.
It feels like change will never come to us. It’s near impossible to get safe supply and we also do not have detox or anything that will help with folk to access recovery without uprooting themselves from their community and leave their families behind I think of all those single mothers that do not have access to that.
We only just got a FTIR spectrometer to test drugs a few years ago, so we did not have the capacity to have a full understanding of what our toxic drug supply level was until recently.
I’ve been doing drug checking since I was 19, and volunteering with ANKORS before then, too. I’m 27 now. I’m terrified, to be honest, to see raves in our area come back because a lot of the folks attending aren’t using every day. They have no idea how toxic it is now. I’m supposed to service all of the East Kootenays, which is very difficult in the middle of winter but I find strength when they’re doing the little things to keep themselves safer. But we’re exhausted, and we’re tired of death.
Our goal is just to make people survive the night and we take it day by day, because it’s hard to do anything else.
Jen St. Denis is The Tyee’s Downtown Eastside reporter. Find her on Twitter @JenStDen. Moira Wyton is The Tyee’s health reporter. Follow her @moirawyton
This article is reprinted with permission from thetyee.ca. Contributions are edited for length and clarity.