 Who is Captain Obvious in our healthcare system?
Who is Captain Obvious in our healthcare system?
By Shirlee Sharkey
I love Captain Obvious. Hotels.com has struck gold by choosing a well-defined and memorable character to promote its brand—and an obvious one, at that. My thanks to the good Captain for helping me with the perfect analogy. Captain Obvious in our Canadian health system is none other than “person– and family-centred care” (PFCC)…obviously.
One definition of client-centred care is “…an approach to the planning, delivery and evaluation of home and community care that is grounded in mutually beneficial relationships and partnerships among people using the health care system, their family and health care providers.”
When you think about it, it does seem obvious that patients and families should be at the centre of their own health care. However, just because something seems obvious does not make it simple to change. It is not that health care providers do not want individuals and families at the centre of their own personal health journeys—we certainly do! Over time, however, systems and processes have been built and have become somewhat like a tree with a complex root system. And, as such, something that seems obvious in today’s context was not obvious in the past.
The great news is that PFCC is taking hold, with this new way of looking at care being implemented in virtually every corner of the system. Technology and the power of people are coming together in a dynamic way to change our approach to care. President John F. Kennedy famously said, “The rising tide lifts all boats.” If we take advantage of these factors, we can all rise and benefit.
The research
At Saint Elizabeth, the majority of the care we provide for clients happens in their own homes. As a result, and unlike in other institutional care settings, our work tends to lean towards a collaborative process with people and families, and unique relationships form naturally. This differentiator has led us to conduct research and develop methodology around PFCC. The research we have done tells us that PFCC is valuable and important. It results in more satisfied clients, and greater patient and family involvement in care. The research also shows that when a PFCC approach is applied, less time is spent managing conflict and staff are more content.
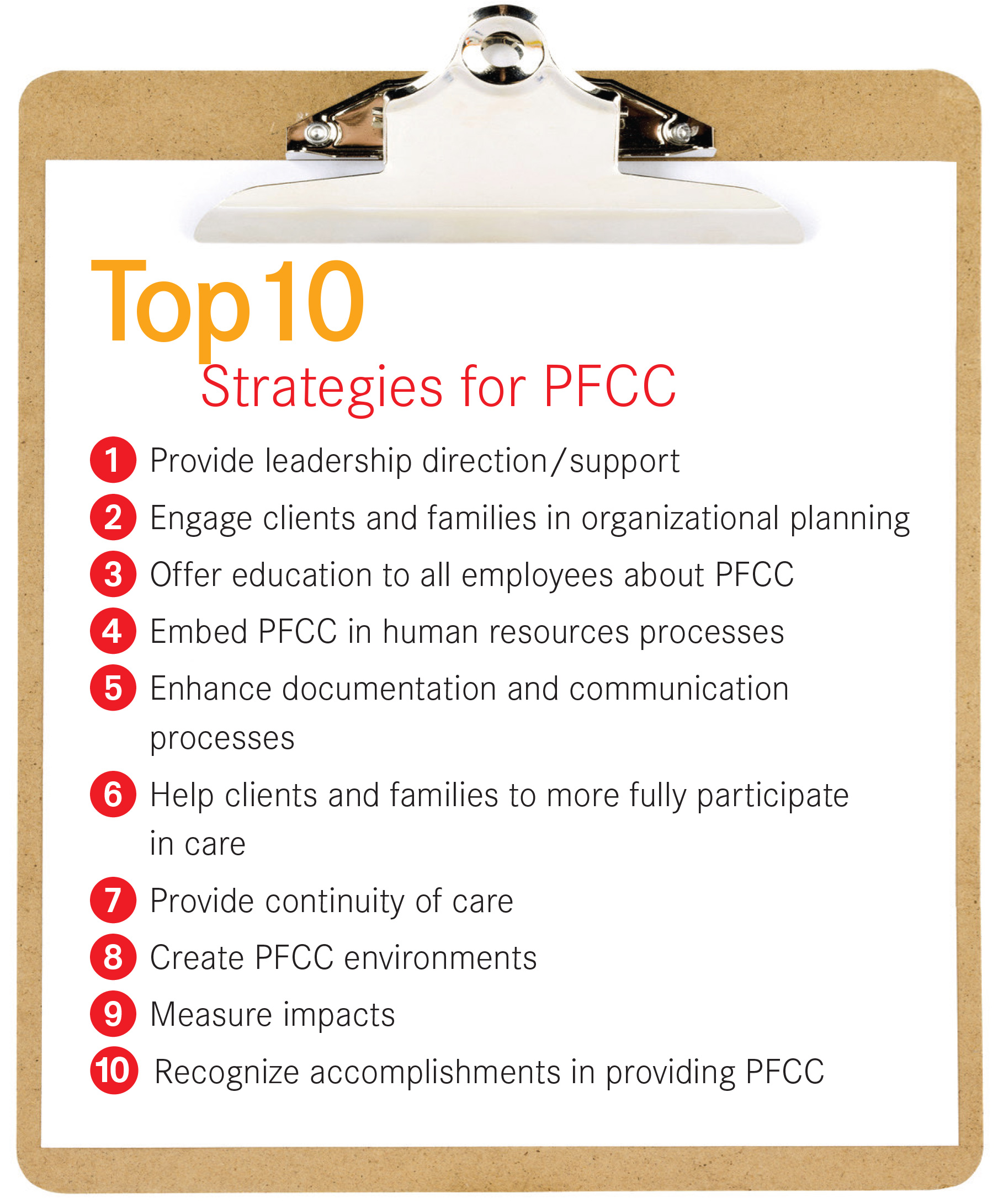
Our own journey has also reminded us of how challenging it is to genuinely implement the principles and practice of PFCC. With that in mind, we have developed strategies and resources to help others embrace and institute this approach. The training we have developed, based on research, will help with new accreditation requirements. We are so pleased to see PFCC taking centre stage.
To make sure we “walk the talk,” we are operating with PFCC goals in mind and it is my commitment that the spirit of collaboration will be evident throughout our organization. To help others, the Saint Elizabeth Research Centre and Education Services are collaborating to make the results of the research available to heath care organizations across the country through free resources, as well as through education and consulting services.
Technology
Technology is a tremendous tool that is driving and shaping PFCC. Embracing technology that works for people and providers is critical to truly implementing PFCC. There is currently a buffet of innovative technologies that can inexpensively supplement and enhance care—from communication platforms that facilitate virtual visits and monitoring, to smart homes and the emerging internet of things. With advances in technology, the physical location of people and providers is becoming less relevant. Individuals are already using all of these forms of technology in their day-to-day lives. As advocates of PFCC, we want to leverage these technologies to bring people together.
 Technology can also be an enabler when we consider rethinking our basic tools (e.g., our assessment approaches, documentation, how we set care goals, how we organize our space, how we set our work schedules and how we relate to one another) and so there is lots of room for work within organizations—and for collaboration across the health care system.
Technology can also be an enabler when we consider rethinking our basic tools (e.g., our assessment approaches, documentation, how we set care goals, how we organize our space, how we set our work schedules and how we relate to one another) and so there is lots of room for work within organizations—and for collaboration across the health care system.
The power of people
PFCC is a perfect fit in today’s environment. Empowered consumers, armed with information and used to customization in their day-to-day lives, are ready for us. As health care professionals, it is not about us trying to get uptake on a new behaviour; rather, it is about letting it happen. PFCC invites people to be involved—to make choices and plans, and to collaborate in their own care.
But achieving PFCC is hard work. Even those who are passionate and committed towards the approach realize that it is a long journey. Because PFCC is so individual, each setting (e.g., home, community, rehabilitation, acute care) comes with its own set of unique applications. And because PFCC is not a one-size-fits-all practice, it does take commitment, learning and patience to implement and for it to permeate throughout an organization.
Living and breathing PFCC has a great benefit for staff. It enables more personal and professional fulfillment. The results are happier staff; better outcomes; stronger relationships; and a health system that is supported wholeheartedly by clients, families and providers—it provides the best that people and technology have to offer.
Shirlee Sharkey (@ShirleeSharkey) is the President and CEO of Saint Elizabeth. For more information on PFCC, including free resources and toolkits, please visit www.saintelizabeth.com.
Photo: Hotels.com













